Provider data governance is a complex topic. It includes the people, processes, and tools you need to ensure that your healthcare payer organization is as much value as possible out of your provider data. However, there are some key mistakes that can keep you from getting the most out of your governance processes. In fact, some of these can render your programs virtually useless if you don’t address the issues quickly.
Not Having a Provider Data Governance Program
The very first mistake is not having a governance program in place at all. Health plans that operate without a clearly defined Provider Data Governance Program (PDGP) are basically living in the Wild West. Data is flying everywhere, landing where it may, and without regard to whether it’s accurate or not. In these situations, you’re relying on a handful of knowledgeable individuals within the organization to manually monitor the data. Your staff plays Whac-a-Mole with issues that arise. They never quite get their work queues clear. Problems fester and complaints from members and providers rise.
Health plans without a PDGP often experience nearly all of the adverse effects of poorly managed provider data. Claims don’t get paid correctly and are often late. Provider directories are incorrect. This leads to member complaints and voluntary disenrollments. Clinical teams have a difficult time getting referrals and authorizations processed. Reporting becomes nearly impossible due to the data issues. System implementation and migration projects may stall and fail.
If you don’t have an effective governance program in place, the best time to start is today. Virtually anything is better than nothing at all. Developing your PDGP is a journey – the sooner you take the first step, the sooner you start to benefit.
The Wrong People Are Leading the Program
As with any endeavor, it’s important to get the right people on the bus. Then you need to get them in the right seats. This might be the most difficult phase of developing your program. It’s important to emphasize that you need the right people leading this initiative.
The tendency might be to assign an analyst from Provider Operations as the data steward. Alternatively, you might assign someone from your technology team. The person’s specific role and where they sit in the organization matters less than their competencies. Ideally, you want someone who is data-savvy. They should be able to understand the complexities of provider data models within a health plan.
However, your lead data steward should also understand the business needs in great depth. They should be well versed in the challenges on the front lines. Their role should have them interacting with leaders from across the organization on a regular basis. As a result, they need the ability to understand complex technical concepts but communicate in clear business terms with their constituents.
Take your time staffing the effort. It’s success depends on it.
Stakeholders Are Left Out
We need the right people leading your provider data governance program. But at the same time, we need the right stakeholders to be engaged in the process as well. Most of these stakeholders will be internal to your organization. Some of them should come from outside of the organization as well.
Internally, provider data impacts nearly every business unit within your plan. At a bare minimum, you’ll need to engage Claims, Utilization Management, Enrollment, Customer Service, and IT. You may have downstream constituents in Finance, Medical Economics, or a Data Science unit. It may be helpful to define each business unit that is impacted. Then, use a rating system to determine how involved each group should be in the provider data governance process.
Your external stakeholders will likely have less involvement. Their voices are still important, so don’t ignore them. These stakeholders are likely from your major contracted medical group and health networks. Ideally, your contracts and provider manuals should outline expectations and processes for how they communicate with your team. (Think about the No Surprises Act, for example.) Getting their input to understand their capabilities and constraints is a key part of the governance process.
Members may be engaged to the extent that you want to understand whether your provider data is supporting their needs. Is your provider directory easy to navigate? Was the information in the directory helpful and accurate? What could be done to improve it? You may leverage customer service, surveys, or focus groups to get this kind of feedback.
Provider Data Quality Auditing is Lacking
Any governance process that doesn’t include rigorous quality assurance and improvement processes is only partially complete. How will you know if you’re moving in the right direction? How will you identify and address root cause issues? Without comprehensive data quality management, you’ll be searching in the dark. It’s likely only slightly more informed than the Whac-a-Mole approach we discussed earlier.
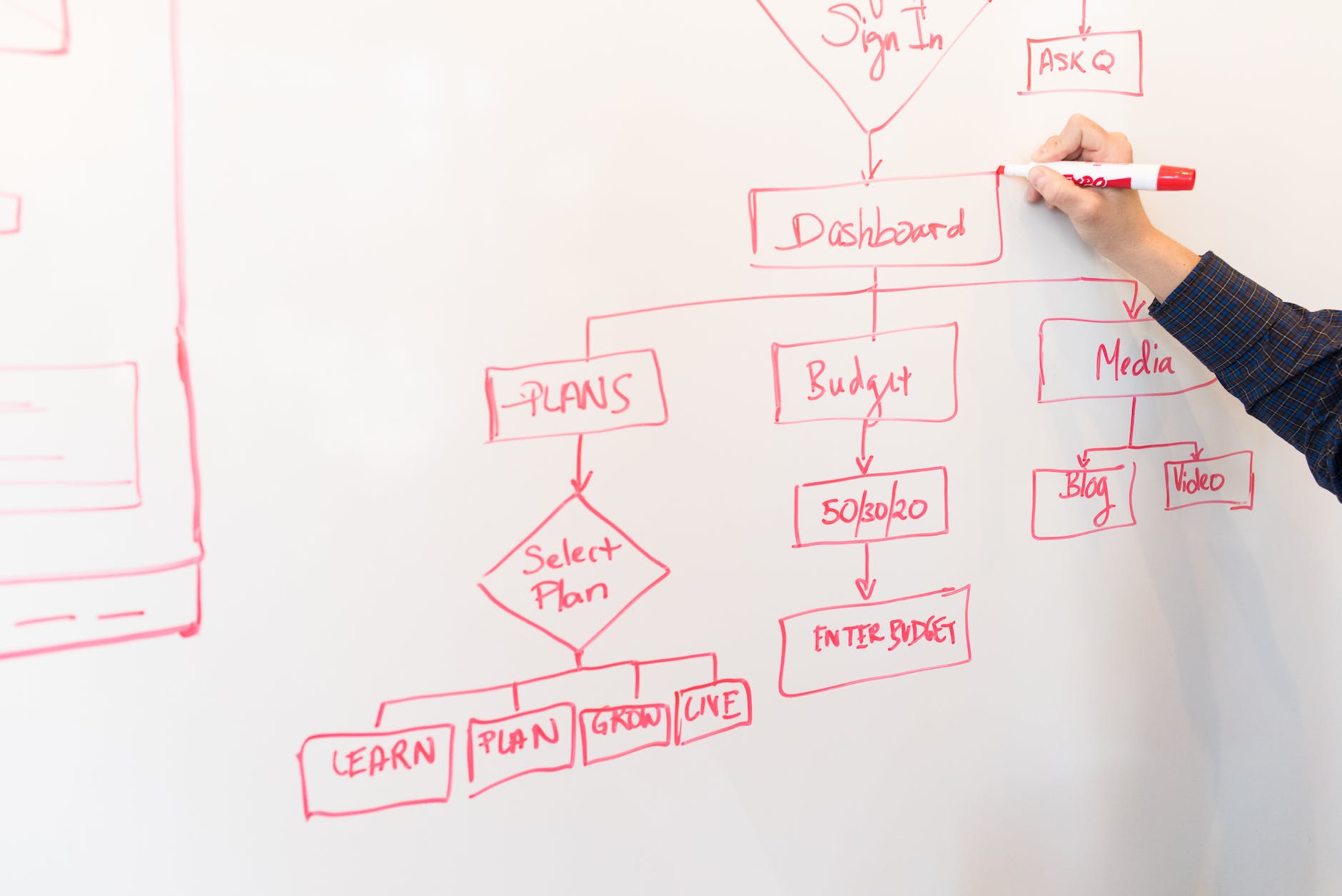
At a bare minimum, your governance team should develop a set of dashboards that get reviewed on a fixed schedule. The dashboards should highlight KPIs from the governance program and indicate whether you’re meeting or missing those. You should have the capability to monitor over time. Provider data is fluid and if you begin to regress, you’ll want to be able to pinpoint when and where it began.
Dashboards can be built off of an existing data warehouse using basic tools like Tableau or PowerBI. (You can also leverage Maven One Rules Engine to perform the quality analysis and visualize your performance.) Once deployed, it’s important that individuals within your provider data governance team be responsible for monitoring those dashboards routinely.
The expectation should be that they investigate anomalies and missed KPIs for root causes. They should also be empowered to work with stakeholders to address root causes. This might include system changes, process changes, or recommending training and refreshers for front line staff.
Continuous Improvement in Provider Data Governance
These are just a few of the key issues that can arise in the journey to building an effective PDGP. Keep in mind that this is a process in and of itself. It won’t be perfect over night. And as soon as you feel that you have it dialed in, a new hurdle will arise. Change is the nature of our world. A mindset of continuous improvement will go a long way toward ensuring that your organization is getting the most out of the process and the data it oversees.